When the COVID-19 pandemic began, the use of telehealth skyrocketed. US Census Survey data shows that 22 percent of Americans made use of telehealth services in 2022. With more than 1 in 5 patients having engaged in telehealth, the American population is now familiar with the concept of a basic virtual doctor visit. While the Biden administration recently ended the COVID National Emergency, the pandemic has resulted in many changes to our everyday lives, including how we work, shop and access health care services.
“It’s created such a powerful help to our clinicians and patients and many different settings,” said Dr. Gokhan Anil, the Regional Chair of Clinical Practice for Mayo Clinic Health System (MCHS). “The pandemic’s urgency was great when we had to shut down the services that patients are very much used to seeing their providers in person,” said Dr. Anil. “This was a huge necessity.”
Dr. Anil believes telehealth is here to stay, and he and his colleagues at Mayo Clinic are looking at innovative ways of providing patients with the care they need. Dr. Anil acknowledges that human contact is always going to be an important component of medical care. However, he argues that telemedicine, telehealth, and digital healthcare should be expanded to make healthcare more accessible, especially for patients in rural areas who often don’t have access to specialists. Increasingly, video visits are covered by medical insurance and third-party payers at a rate similar to in-person appointments.
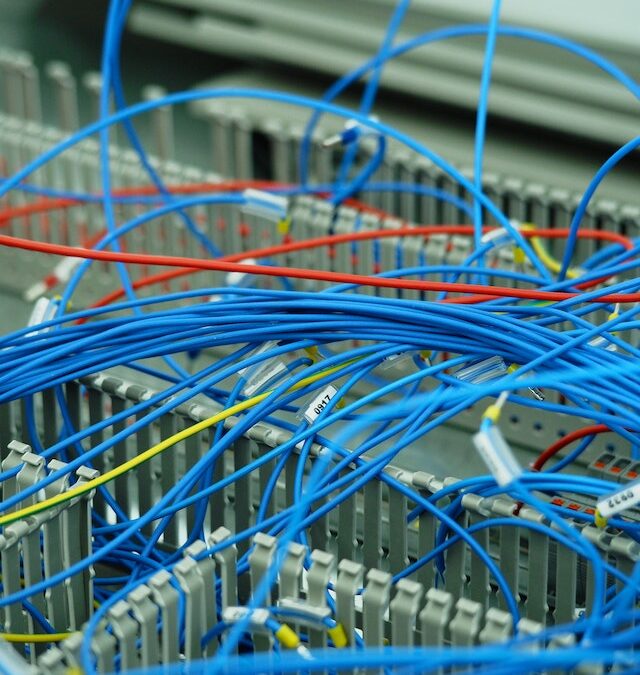
Broadband Is Key to Telehealth’s Access
The Mayo Clinic Health System, which provides health care services to rural communities, is currently incorporating telehealth into its offerings to help reach populations living in remote areas of the country, Dr. Anil explains. But to do this effectively, these communities need access to broadband Internet services. This is why the Mayo Clinic Health System is encouraging the government to provide broadband access in rural communities.
There are currently many mobile healthcare apps available on app stores as well as other health-related web content available online. However, accessing these digital resources as well as telehealth services typically requires access to broadband Internet and a compatible electronic device. The following three pilot telehealth programs assess the impact of broadband adoption:
1. Increasing Healthcare Access in Urban Communities
Chattanooga, Tennessee is using its urban broadband network to support telehealth accounts for residents of Orchard Knob, an under-resourced neighborhood in the city. The project is being coordinated by Enterprise Center, a nonprofit organization that focuses on technology and inequality, in partnership with Parkridge Medical System.
Neighborhood residents experience abnormally high levels of asthma, diabetes, heart disease, and stroke. Area jobs don’t typically offer medical insurance, yet many residents working these jobs don’t qualify for government health programs because their income is too high. Enterprise Center is providing home Internet, accessible devices, and digital skills training. They are supported by the city’s electric power board, which not only funded the project but will power the accounts and will be providing free Wi-Fi in public places.
2. Providing Virtual Mental Healthcare Services
Kansas City, Missouri, delivered family mental health services to one of the city’s most economically distressed communities via telehealth. This project was coordinated by Essential Families, a nonprofit organization. Besides providing mental healthcare services to community families, it also offered virtual parental education to improve parenting skills.
3. Providing Healthcare Access to Rural Communities
Another pilot project coordinated by wireless ISP Vistabeam oversaw the launch of an Empowerment Center in Torrington, Wyoming. The center helps eligible residents enroll in the Affordable Connectivity Program, provides digital skills training, and facilitates video conferencing. A digital navigator is available onsite full-time.
Vistabeam also partnered with a telehealth company to pilot a medical suite that offers a range of health monitoring capabilities. These include a blood pulse oximeter to measure blood oxygen levels, blood testing, and blood pressure checking. The center will also offer private space and resources for residents to access remote telehealth visits.
Providing rural communities with access to broadband Internet and telehealth services is just one component. Having an entity that can coordinate these resources and help patients connect with the appropriate healthcare professionals is essential to the success of these programs. But as Matt Larson, owner of Vistabeam, points out, “the quality of broadband infrastructure is key to telehealth success—it cannot fail customers!”